A deadly fungal infection is rapidly spreading through hospitals across the United States, raising alarms among health officials. Candida auris, a fungus first identified in 2009, is making a dramatic comeback with a staggering spike in cases in recent years. Once a rare occurrence, C. auris infections are now emerging at an unprecedented rate and in more varied forms than ever before.
Candida auris Declared a Top Threat in US Hospitals
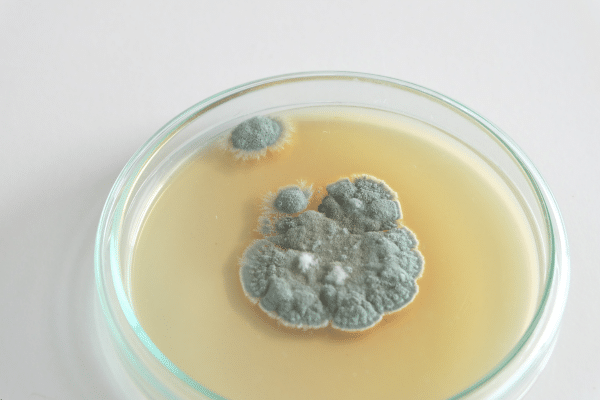
According to the Centers for Disease Control and Prevention (CDC), Candida auris is now officially classified as an “urgent antimicrobial resistance threat.” First reported in the US in 2016, the fungus is known for its ability to resist traditional antifungal treatments and withstand common disinfectants used in hospitals.
Health systems are under mounting pressure to adapt quickly. A recent focus on one major hospital network in Miami, Florida, revealed an alarming trend. Infections in that system surged from only five reported cases in 2019 to 115 in 2023. That 2,200 percent increase has raised urgent questions about the fungus’s rapid spread and its evolving ability to survive typical containment methods.
Hospitals Struggle to Contain a Stealthy Invader
The Miami-based study observed a sharp increase in clinical cultures testing positive for C. auris in 2020 and 2021, followed by a continued but slower rise in 2022 and 2023. Hospital-acquired infections appear to be the primary source of transmission, with the fungus often spreading through catheters, feeding tubes, and breathing equipment. These environments make it easier for C. auris to jump from patient to patient.
Compounding the concern, many strains of C. auris are resistant to standard antifungal medications and fail to respond to conventional hospital-grade disinfectants. That makes containment especially difficult in intensive care units and other vulnerable hospital wards.
The Hidden Danger: Who is Most at Risk?
Despite the alarming numbers, Candida auris does not currently pose a major risk to the general population. Most healthy individuals are unlikely to encounter or be affected by the fungus. However, patients already hospitalized or those with compromised immune systems face far greater risk.
In these high-risk groups, C. auris can cause life-threatening infections. Bloodstream infections remain the most commonly reported, but infections in soft tissue, bones, and even cerebrospinal fluid are becoming more frequent. This expanding range of infection sites makes detection and treatment far more complicated for healthcare providers.
A Growing Global Health Crisis
While the spotlight is currently on the US, C. auris is far from a local issue. Countries across the globe have been grappling with outbreaks for over a decade. Health systems worldwide are now facing similar challenges, including drug resistance and difficulty in preventing the spread within medical facilities.
The fungus was first discovered in Japan in 2009 and slowly made its way across international borders. By 2016, it had reached the US, and within a few years, half of all US states had reported at least one case. Despite numerous alerts from infectious disease experts, the threat continues to grow.
CDC Responds With Urgent Infection Control Guidelines
To curb the spread of Candida auris, the CDC has released detailed guidelines for hospitals. The key recommendations include the use of single-patient rooms, rigorous cleaning procedures, and early detection protocols. Hospitals are also being urged to isolate infected individuals and implement strict contact precautions to minimize transmission risks.
According to the research team behind the Miami study, early identification of patients colonized with C. auris could dramatically impact infection rates. Rapid response and immediate deployment of prevention strategies remain the most effective defense against further outbreaks.
“Measures to prevent the spread of C. auris rely on isolation and contact precautions,” the researchers wrote. “Our findings suggest that early identification of patients colonized with C. auris and the prompt deployment of infection prevention strategies can potentially impact the incidence of bloodstream infections.”
A Race Against Resistance
The challenge posed by C. auris lies in more than just its rapid spread. It is the fungus’s resistance to treatment and cleaning agents that makes it particularly dangerous. Hospitals may not even realize they are dealing with an outbreak until it is already widespread. The longer it goes undetected, the harder it becomes to control.
With infections now appearing in multiple body systems and medical environments, the fungus is proving to be adaptable and persistent. That adaptability presents a serious concern for long-term healthcare management.
Urgency Mounts as Numbers Continue to Rise
The findings from Miami paint a concerning picture of what may lie ahead for other regions. If not addressed quickly, other cities and health systems could see similar explosions in infection rates. The need for vigilance, rapid response, and strict adherence to CDC guidelines has never been greater.
As hospitals nationwide confront this growing threat, the message from health officials is clear. Candida auris may not be a household name yet, but its impact is already being felt where it matters most—in the places where lives are most vulnerable.
Stay Updated with Breaking News
Get real-time updates on breaking stories, trending topics, and the latest headlines. Follow Dumbed Down News on X (formerly Twitter) for fast, no-nonsense coverage!
Click here to follow now: Dumbed Down News


