A surge in emergency room visits tied to popular weight-loss medications has raised new concerns about their side effects. Between 2022 and 2023, nearly 25,000 hospital visits were linked to semaglutide, the active ingredient in Ozempic and Wegovy, according to new health surveillance data. The majority of these cases occurred in 2023, underscoring the need for increased awareness around the risks of these widely used medications.
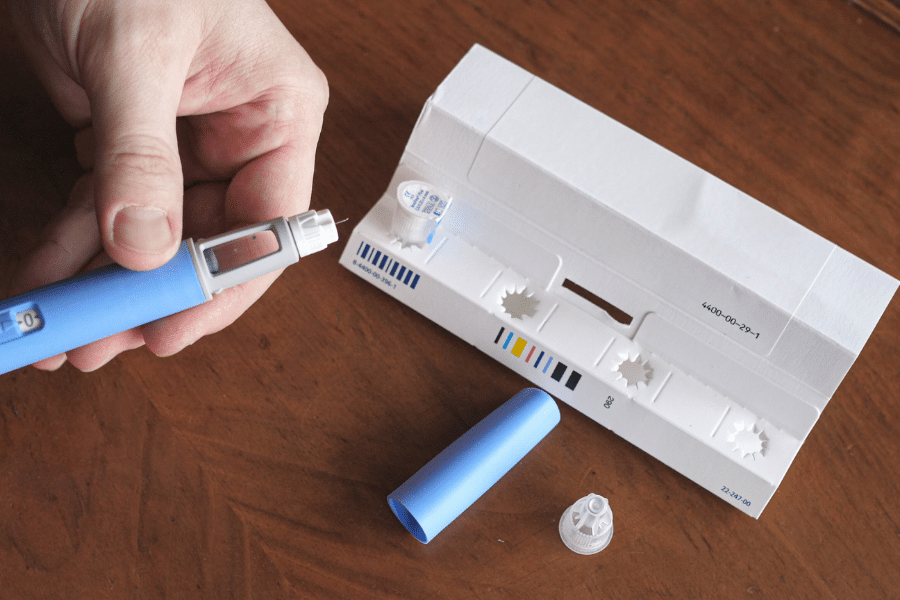
These drugs, originally developed to treat type 2 diabetes, have seen a dramatic rise in popularity for weight management. As of early 2024, it is estimated that one in eight adults in the United States has used a GLP-1 medication, with Ozempic and Wegovy leading the charge. Marketed as once-weekly injections that help regulate appetite by affecting brain signals linked to hunger and satiety, these medications have quickly become household names.
However, the rise in their use has coincided with a growing number of adverse reactions. Researchers analyzing national hospital data discovered a sharp uptick in emergency room visits related to semaglutide use. Over 82 percent of these incidents took place in 2023 alone, pointing to an alarming trend as more Americans turn to prescription weight-loss drugs.
The most frequently reported complications were gastrointestinal in nature. Patients experienced severe nausea, persistent vomiting, abdominal pain, and diarrhea—conditions serious enough to warrant urgent medical attention. These symptoms align with the commonly known side effects of semaglutide, but their severity in many cases was unexpected and debilitating.
Medical professionals also documented a range of less common but significant side effects. These included episodes of low blood sugar, allergic reactions, pancreatitis, and bile duct disease. While these issues occurred less frequently, their presence highlights the importance of careful medical supervision when using GLP-1 receptor agonists.
Experts stress that these are not newly discovered risks. Dr. Pieter Cohen, associate professor of medicine at Harvard Medical School, emphasized that although rare, these adverse events can be severe enough to require hospitalization. He noted that clinicians need to remain vigilant and communicate these risks clearly to patients before starting them on the drug.
Supporting this viewpoint, Dr. Mahyar Etminan, associate professor of medicine at the University of British Columbia, stated that most of the side effects highlighted in recent findings are already listed in product information. However, he agreed that they deserve renewed attention due to their growing impact on hospital systems.
Healthcare providers are being urged to implement safeguards when prescribing semaglutide. This includes adjusting other medications to reduce the risk of hypoglycemia and ensuring patients are aware of potential gastrointestinal complications. Proactive counseling can reduce unnecessary hospital visits and improve patient outcomes.
More severe concerns have also emerged over time. In June 2024, semaglutide was linked to cases of gastroparesis, also known as stomach paralysis. This condition prevents the stomach from emptying properly and can severely disrupt digestion. Later in September 2024, the U.S. Food and Drug Administration (FDA) issued a formal warning about the risk of ileus, a life-threatening bowel obstruction that can cut off blood flow and lead to tissue death if not promptly treated.
Despite these reports, the manufacturer of Ozempic, Novo Nordisk, stands by the drug’s safety profile. In a statement, the company reiterated that the risks associated with the medication are well documented and reflected in the FDA-approved labeling. They maintain that when used as prescribed, the benefits of semaglutide outweigh the potential downsides.
Still, the conversation around these drugs continues to evolve. While millions have successfully lost weight using GLP-1 medications, the emerging pattern of hospitalizations suggests the need for a more cautious and informed approach. Doctors are being called to better balance the promise of rapid weight loss with the reality of potential complications.
The explosive growth of the weight-loss drug market shows no signs of slowing. As more people seek quick and effective solutions to obesity and related conditions, medical professionals must remain proactive in managing risks. Monitoring patient responses, adjusting treatment plans, and educating users about possible side effects will be essential in preventing hospital emergencies linked to these medications.
While the number of severe incidents remains low relative to the total number of users, the nearly 25,000 hospital visits serve as a warning. These medications are powerful tools but must be used with respect, oversight, and a clear understanding of the risks involved.
Stay Updated with Breaking News
Get real-time updates on breaking stories, trending topics, and the latest headlines. Follow Dumbed Down News on X (formerly Twitter) for fast, no-nonsense coverage!
Click here to follow now: Dumbed Down News